Visualising your diabetes data can really help you to gain insights to intervene and gain greater control of your diabetes. There are tools out there than can help. This issue, it’s insulin pumps and CGM, next issue we look at blood test meters and more.
Visualising your diabetes data can really help you to gain insights to intervene and gain greater control of your diabetes. There are tools out there than can help. This issue, it’s insulin pumps and CGM, next issue we look at blood test meters and more.
Pump screens, CGM receivers and smartphone apps can help you track your glucose levels and insulin ‘on board’, as well as trends in your levels with arrows and alerts telling you if you are going up, or going down. With that info, you can take a view: pip in a little more insulin, have a biscuit, put on a temporary bolus. It helps you take action before you’re too far up or down.
The following is a brief overview of what is available and it’s specific features and benefits. The first are CGM systems, the last is Flash Glucose Monitoring, which is slightly different (see glossary). This feature is intended as a guide as to what is available, not as advice as to what is best for your individual healthcare. For that you should speak to your healthcare professional for advice.
Company: Dexcom
Product: G5 CGM
Screen: Receiver or smart phone
This is a stand-alone system that works closely with some of the current insulin pump systems, particularly Animas pumps and the Omnipod system. With quite a fan-base, Dexcom users claim it’s not only accurate but easier to wear than other CGM options.
Following the decision by Johnson & Johnson to cease to support insulin pumps globally withdrawing its popular Animas pump in the UK as well as elsewhere, when it comes to choosing their next pump at their next pump change, Animas users may decide to move over to a pump that also incorporates Dexcom to keep that continuity
With a relatively newly formed UK company, Dexcom is starting to make greater in-roads across the country seeking to broaden the user base out beyond those already on an insulin pump.
The positive impact of CGM for diabetics on injections was shown via the DIaMonD study (Multiple Daily Injections and Continuous Glucose Monitoring in Diabetes), the first-of-its-kind study that demonstrated the impact of CGM on HbA1c and hypoglycaemia in participants on multiple daily injections (MDI).
Published in January 2017 in Journal of the American Medical Association (JAMA), the study showed Dexcom CGM System users on MDI achieved a 1% average reduction in HbA1c after 24 weeks of regular use. In addition to better glucose control, participants also increased time spent in target range and spent less time in hypo and hyperglycemia when they used a Dexcom CGM system, compared to those who used only a standard meter to monitor their glucose. There was a 49% reduction in time spent in hypo (less than 3.9 mmol/L). The study also dispelled certain perceptions, such as CGM being too complicated to use, as patients demonstrated significant HbA1c reductions regardless of education level, maths ability, or age. A high level of adherence was also achieved with 93% of patients still using the Dexcom CGM system more than at the end of the study.
Company: Medtronic
Product: CGM, Enlite sensor
Screen: Insulin pump (MiniMed 640g)
Medtronic’s CGM uses an Enlite on-body glucose sensor with transmitter that sends readings into its MiniMed 640g insulin pump every five minutes (so 288 times a day). The MiniMed 640g insulin pump system includes an array of alarms that can be adjusted around an individuals needs and which have been proven to increase time spent in range.
The insulin pump’s screen shows the data as a line, with pre-set high and low levels helping people to see how much time they have spent in range. Increased time in range has been linked to improved HbA1c outcomes.
Medtronic’s SmartGuard technology operates on it’s MiniMed 640g insulin pump systems, incorporating ‘suspend before low’, whereby the pump is enabled to suspend insulin delivery when sensor readings are predicted to go below a set level. This has been proven to greatly reduce – and even eliminate – hypos, especially at night, giving users greater confidence in trying to keep glucose readings in range and thereby leading to greater overall control
Suspend before low is one half of the equation, with the next-generation MiniMed 670g insulin pump system (only currently available in the US) also having the ability to increase insulin basal rates at a set level if glucose readings are high.
Company: Medtronic
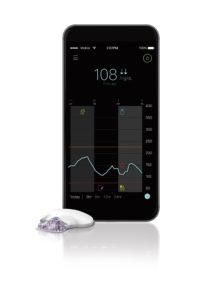
Product: Guardian Connect CGM
Screen: Smartphone app
Medtronic also now has a new stand-alone CGM option. Medtronic’s Guardian Connect is mobile continuous glucose monitoring (CGM) system for people with diabetes using insulin injection therapy.
With Guardian Connect, people on insulin injections are able to check their current glucose level anytime on their mobile device, as easily as checking other information sources such as email, the weather or social media. Users can also be alerted of high and low glucose levels on their mobile device, helping them confidently avoid or address high and low glucose situations.
Guardian Connect is the first and (currently) only mobile CGM system with customizable SMS text alerts that enable care partners (parents, spouses, carers) to receive high and low glucose alerts on any connected mobile device. The system also features the option to automatically upload the data daily into Medtronic’s CareLink therapy management software. That reduces the burden of data upload for both people on multiple daily injections (MDI) as well as their healthcare providers.
“Having continuous, real-time access to glucose values and being alerted to important trends and events is key for people with diabetes. With our new Guardian Connect system, we’ve continued to innovate so we can deliver these insights for people with diabetes on insulin injection therapy,” says Annette Brüls, president, Diabetes Service and Solutions at Medtronic. “Guardian Connect is also compatible with our CareLink diabetes therapy management platform and arms healthcare providers, their patients and care partners with actionable data to help improve day-to-day diabetes management and make long-term therapy adjustments.”
The Guardian Connect system consists of a small wearable CGM device that takes glucose readings every five minutes (288 times a day) and sends these glucose values directly to a smartphone app. People on insulin injection therapy can use the system to check glucose levels on their mobile phones, enabling them to see highs and lows in real-time, understand the trends and help improve their daily management of diabetes. Healthcare professionals can leverage automatic daily data uploads via CareLink.
The Guardian Connect smartphone app will initially be available with iOS devices. Medtronic is currently developing an Android version of the Guardian Connect app for release at a later date.
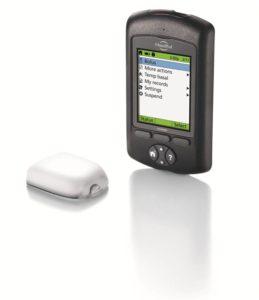
Company: Insulet
Product: Omnipod
Screen: Personal Diabetes Manager (PDM) handset
Omnipod’s clear advantage is that it does not having any tubing, the insulin is in an on-the-body pod which delivers it following preset basal and wireless instructions for bolus doses from the Personal Diabetes Manager (PDM), a handset which doesn’t need to be worn and comes with an integrated blood glucose meter and bolus calculator. The two parts – the pod and the PDM – are simple and lightweight. Some might worry about wearing a pod on the body, but most users do not revert back to tubing having tried Omnipod, also referred to as a patch pump. Note, the pod (which is worn for up to three days) is waterproof but the PDM is not.
UPDATE
Insulet Corporation is in the process of establishing direct operations for its Omnipod System across Europe. That means that the company will be taking over the distribution, sales, marketing, training and support for the Omnipod System across Europe once its agreement with Ypsomed ends at the end of June 2018. The two companies will work closely to ensure continuity of care for Omnipod users. In the UK, the Omnipod System is the same product as mylife OmniPod but has always been manufactured by Insulet. Current users can be assured that this transition will not affect the supply of your Omnipod products with Ypsomed continuing to operate as the point of contact during the transition period. You will be given advance notification of any changes to the ordering process to ensure continuity of care. Check this website for the latest information and updates: www.myomnipod.com/europe
Company: Roche Diabetes Care
Product: Accu-Chek Insight insulin pump
Screen: Accu-Chek Insight handset
In the Accu-Chek Insight insulin pump the introduction of wireless transmission of blood glucose data immediately led to an increased use of bolus calculator by users, as well as an increased adjustment of therapy via the on-screen manager. Easier to use than previous models and more ‘visual’, users are able to quickly see an overview of their diabetes control. The training for using the pump is short. As the handheld unit is just like a smartphone, people quickly pick up how it works. It’s a touch-screen and in colour and presents an immediate display of data in colored tables and graphs on the Accu-Chek Aviva Insight diabetes manager handset.
Enhanced data management functions facilitate communication with healthcare teams by means of a fully synchronized diary which stores blood tests, insulin dosages and information on meals and activities as logged by the user. Two-way Bluetooth interface enables safe communication between the two main components of the Accu-Chek Insight system (the pump and the manager handset). An intuitive user interface on the colour touchscreen of the handheld offers full control for daily diabetes life. It is discrete and private to use via the remote control and the pump incorporates an easy to use pre-filled cartridge system

Senseonic’s Eversense CGM (on left), reader (center) and smartphone app screen right) distributed by Accu-Chek Roche in the UK.
Company: Roche Diabetes Care
Product: Eversense implantable CGM
Screen: Eversense Mobile App
The Eversense implanted CGM system continually measures interstitial fluid glucose levels in adults with diabetes for the operating life of the sensor, which is currently indicated at 180 days (six months). Although the CGM is implanted the user wears a reader on the skin above the technology. The data received and viewed via a smartphone app includes glucose trend information and alarms for the detection and prediction of episodes of hypo and hyper. The aim is that the system will allow users to manage their diabetes with more flexibility, confidence and discretion. The system needs calibrating twice a day with a blood glucose reading. The Eversense sensor is inserted in a clinical environment where a 5‒8 mm insertion is made in the upper arm under a local anaesthetic). A small pocket is then created 3‒5 mm under the skin into which the sensor is inserted using a special insertion tool. The insertion is then closed with steri-strips.
The implanted sensor is powered wirelessly by the transmitter placed on the arm directly over the sensor. The Eversense mobile app can send the data wirelessly to a cloud-based application allowing the data to be shared with the caregiver or diabetes healthcare team. The sensor is removed in the clinic using local anaesthetic. Another sensor can then be inserted into the same place. Alternatively, the incision is closed using steri-strips if a new sensor is to be inserted at a fresh location.
The smart transmitter provides on-body vibration alerts even the smartphone is not nearby or switched off. The Eversense mobile app displays the sensor glucose data from the smart transmitter, displaying the current glucose value every 5 minutes and displays where the glucose is headed and how fast.
Company: Abbott
Product: FreeStyle Libre
Screen: Receiver
Flash Glucose Monitoring is a new category of glucose monitoring designed as an affordable and easy way to generate the amount of glucose data needed for an insightful glycaemic picture. It comprises an on-body sensor but no transmitter. To pick up the data, the receiver needs to be swiped over the sensor. Or, there is now also smartphone apps that do the same thing )see below). What makes flash glucose monitoring unique is this quick scan of the reader over the sensor to collect glucose data. Another key feature of the flash glucose monitoring system is the small and fully disposable sensor that lasts up to 14 days and that automatically measures, captures and stores glucose data. FreeStyle Libre system is designed to be an easy-to-use and broadly accessible device to many patients with diabetes. FreeStyle Libre system is clinically proven to decrease all measures of hypoglycemia in both Type 1 and Type 2 diabetics as shown in IMPACT and REPLACE randomized clinical trials. Data from more than 250,000 people wearing FreeStyle Libre sensors in the real-world (not just in clinic test circumstances) that shows a correlation between more scanning and a decrease in hypos and overall improved control.
UPDATE
A FreeStyle LibreLink app is now available on iOS for iPhones. Previously available on Android smartphones, the FreeStyle LibreLink app is available for iPhone 7 and upward. Using the FreeStyle LibreLink app on a smartphone includes several updates and new features in comparison to the reader including: a larger, high-resolution display, text-to-speech capabilities for glucose readings and the ability to log smaller doses of insulin (0.1 unit vs 0.5 units). The FreeStyle LibreLink app has been launched as part of Abbott’s Digital Health Solutions. There is a list of compatible smartphones available on Abbott’s website.
EDITOR’S COMMENT: Your world in your hands
Always speak to your healthcare professional for advice about these forms of diabetes kit, although at this point, you may not get funding for these technologies from the NHS. However, there’s nothing to stop you asking about how to go about getting it. And for those who can afford it, all are available to be ‘self-funded’ (i.e. buy it yourself). In a culture where we expect our healthcare to be provided by the NHS
While CGM can claim greater impact on HbA1C and time in range than Flash, Flash can claim the same above self-monitoring using blood testing (SMBT). And while it’s more expensive than SMBT, it’s more affordable than full CGM.
And a note about ‘alarm fatigue’. You can always turn the alarms off if you are finding them intrusive. They will be at first, but as you get used to using CGM with alarms you end up with better control, and therefore fewer alarms. You can turn the sensor off if you need to. It’s your call – you may need your sleep (for example) more than you need to know if you are running a bit too high or low). Or, you may feel that an early warning about a hypo is worth being woken for. Start off by setting alarms with a wider range. Once greater control is achieved, these can be tightened up.
Like weight-loss, a little bit of success on easier goals can motivate you to move further with your actions. – Sue Marshall, editor, Desang Media
GLOSSARY
Continuous Glucose Monitoring (CGM)
A CGM system provides continuous, real-time trend information about glucose levels for people with diabetes. It allows for appropriate intervention (after verifying with an old-fangled blood test) to prevent either high or low blood sugar, maximizing the you spend in your glucose target range. To use a CGM system, the user inserts a tiny sensor beneath the skin, typically on the stomach. The sensor, which measures glucose levels from the fluid under the skin (interstitial body fluid), is attached to a transmitter that sends readings to a wearable monitor or the insulin pump, usually every five minutes. CGM provides a more complete picture than blood testing because it reveals high and low glucose levels that periodic blood ‘fingerstick’ testing might miss.
You may also see it referred to as rtCGM – which is the same thing, the ‘rt’ has been added in to represent ‘real time’, which reflects the idea that the data is beamed out and is therefore current on the screen, as opposed to how Flash Glucose Monitoring works (see below). Note that that as CGM reads glucose in interstitial body fluid, not blood itself, and is therefore around 10-15 minutes behind. So it’s ‘almost real time’. For actual real time, do a blood test.
If worried, in doubt, or feel the need to know what your blood glucose is beyond using a sensor then an old-fashioned blood test is a good way to put your mind at rest as to what your actual blood glucose is.
Flash Glucose Monitoring
This also uses an on-body sensor which does not have a transmitter. Readings are picked up by scanning the sensor with a reader, or a smartphone. Flash Glucose Monitoring is a new category that is designed as an affordable and easy way to glean glucose data using a quick scan of the reader over the sensor. The small and fully disposable sensor lasts up to 14 days and that automatically measures, captures and stores glucose data.
News items and features like this appear in the Desang Diabetes Magazine, our free-to-receive digital journal (see below, or www.desang-magazine.co.uk). We cover diabetes news, diabetes management equipment (diabetes ‘kit’ such as insulin pumps and continuous glucose monitoring equipment) and news about food suitable for a diabetic diet including a regular Making Carbs Count column. We just need your email address to subscribe you (it’s free, and you can easily unsubscribe should you wish to).
<ahref=” https://view.pagetiger.com/desang-magazine/Issue87-Feb18 “target=”_blank”>Open publication